Diagnosing breast cancer
Breast cancer is the most common cancer in women. It is suspected when there is a change in the breast or during a screening. Although many breast abnormalities are benign, any recent abnormality should prompt a consultation with a breast specialist, who will prescribe a radiological assessment and if necessary, a biopsy.
Book an appointment
Clinical examination
Clinical breast examination is a key component of breast cancer screening.
In the absence of known cancer, it is recommended to perform a clinical breast and armpit examination (palpation) every year from the age of 25. This can be done by your gynecologist, your doctor, your midwife or any other health professional trained in this procedure.
It should be done systematically if you notice a change in one of your breasts: palpation of a ball, change in shape or volume, appearance of redness, deformation, folds, retraction of the skin. You should also consult if your nipple changes, gets in more than usual or if you have a discharge.
Mammography and ultrasound
La mammographie
Mammography is an X-ray of the breasts. It is the reference examination for breast cancer screening and allows for the early detection of small, non palpable tumors at an early stage.
The images are interpreted by the radiologists, who look for suspicious abnormalities (nodules, microcalcifications, etc.). Remember to bring your previous X-rays so that the radiologist can compare them with the new ones and identify any changes.

Mammography is classified into 6 ACR categories (American College of Radiology BI-RADS Classification):
- ACR 0 : further investigations are necessary
- ACR 1: normal mammography
- ACR 2 : typically benign findings, which does not require any supervision or additional examination
- ACR 3: probably benign findings. Short-term monitoring (4 to 6 months) is recommended
- ACR 4: suspicious findings: biopsy required
- ACR 5: highly suspicious findings: biopsy required
- ACR 6: biopsy proven cancer
Ultrasound
The use of ultrasound will allow either a more detailed analysis of abnormalities detected by mammography, or to improve the analysis of dense breasts (most often in young women) and to perform targeted biopsies in case of suspicious lesions.
Ultrasound can also be used to explore the axillary areas, identify any suspicious nodes and biopsy them.
Mammography and ultrasound can detect suspicious lesions, but cannot confirm a diagnosis of breast cancer. A biopsy is essential to confirm the diagnosis. It is performed by the radiologist under local anesthesia.
MRI is a complementary examination.
MRI does not replace mammography or ultrasound. It is not a systematic examination, neither for screening nor for the diagnosis of breast cancer.
It is a complementary examination that the doctor sometimes prescribes:
- As part of screening for certain patients at high risk of cancer (genetic mutation).
- In case of suspicion of cancer to help in the diagnosis when standard imaging does not allow to conclude with certainty.
- In case of confirmed cancer to better define the extent of the lesions.
- During treatment, especially in the case of pre-operative chemotherapy.
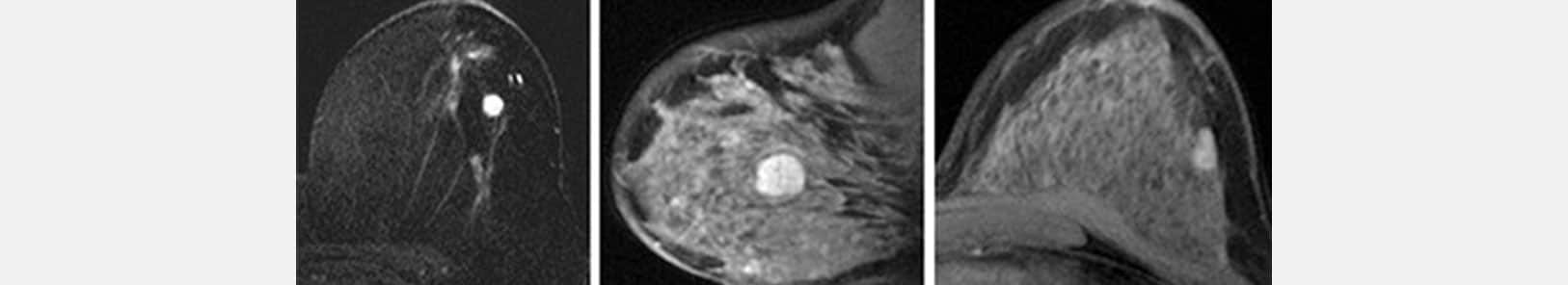
Chez une femme non ménopausée, l’IRM devrait idéalement être effectuée entre le 8ème et 12ème jour du cycle.
Biopsies

A biopsy is a sampling of the suspected area using a needle, under local anesthesia. It is most often performed by a radiologist.
Only a biopsy and microscopic analysis of the suspected area can confirm or refute the diagnosis of a suspicious lesion. In the case of cancer, the anatomopathological examination under the microscope allows to specify the type of tumor and its characteristics.
Microbiopsy is performed with a fine needle under local anesthesia. It allows to take a fragment of the lesion.
Macrobiopsy uses a slightly larger needle and allows for larger and more numerous samples to be taken. It is most often performed on foci of microcalcifications.

The biopsy is guided either by ultrasound, in which case it is called an ultrasound-guided biopsy, or by mammography, in which case it is called a stereotactic biopsy. More rarely, it can be guided by MRI.
Cytopuncture is rather reserved for lymph nodes, it is performed with a simple needle and a few cells are taken.
In some cases, a clip will be placed in the biopsied area. It will serve as a reference for further care.
Pathological examination
Anatomopathological examination under the microscope of the collected tissues is fundamental.
It confirms the diagnosis of breast cancer and specifies the characteristics of the tumor. It establishes a true “identity card” of the cancer, which is essential for the therapeutic choices.
What the pathologist sees

- Macroscopic analysis of the tumor (during surgery)
- Size of the tumor
- Measurement of excisional margins
- Final analysis of the tumor (microscopy, after surgery)
- Confirmation of the size
- Confirmation of excisional margins
- Analysis of the tumor characteristics, which is essential for treatment and prognosis
Tumor genomics
The genetic characteristics of a tumor can be studied through tumor genomics. This is a recent science that helps determine the best treatment to offer.
Tumor genomics makes it possible to study the activity of certain genes in tumor tissue in order to extract personalized information. This information allows treatment to be adapted to each situation.
Genetic testing can be performed on a tumor to assess the need for chemotherapy. There are many different types of tests, with results available in 8 to 15 days. If the genetic test indicates a low “risk of recurrence score,” chemotherapy can be avoided. Conversely, if the score is high, chemotherapy will decrease the risk of recurrence and will be offered.
In situ or invasive cancer?
If the basal membrane is not crossed by the tumor cells, the cancer is said to be “in situ” and is called carcinoma in situ. If the cells are found in the ducts, it is called ductal carcinoma in situ (DCIS), while if the cancer originates in the lobules, it is called lobular carcinoma in situ (LCIS). Lobular carcinoma in situ is not considered a cancer and often does not require treatment (but monitoring is necessary).
In most cases, the tumor cells have crossed the basal membrane. This is called invasive cancer (synonym: infiltrating). About 85% of invasive cancers are ductal cancers, 10-15% are lobular cancers. The remaining cases are rare forms of breast cancer.
Analysis of the tumor margins
After the procedure, the removed area is analyzed by the pathologist. He makes sure that the removal is complete with a safety margin. If not, it may be necessary to operate again.
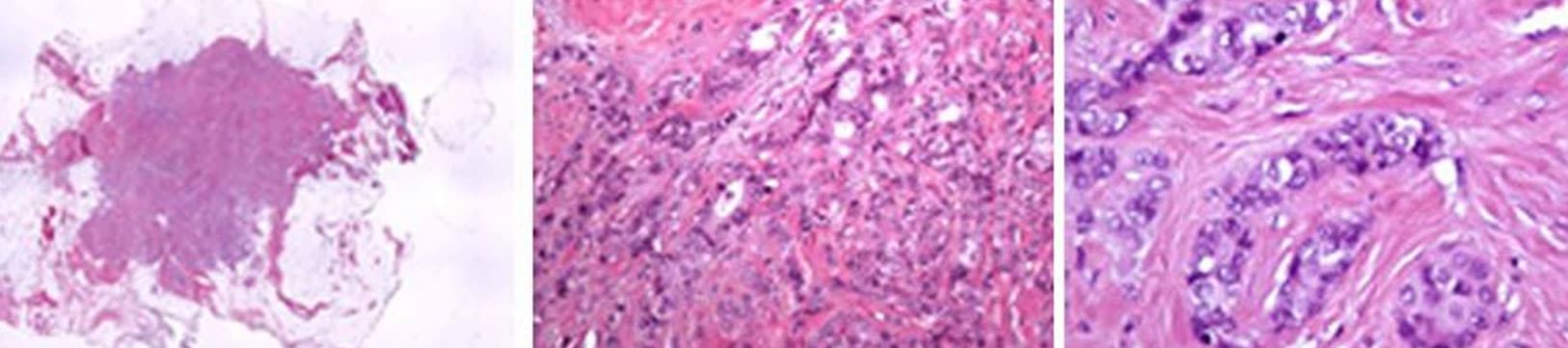
Tumor cell analysis
Depending on the resemblance of the tumor cells to normal breast cells, the pathologist determines whether it is a differentiated or undifferentiated cancer. The more a cancer cell resembles a normal cell, the more differentiated it is (its characteristics are close to those of a normal breast cell), the less aggressive it is.
Based on this and other findings, the pathologist defines the grade of the cancer (called the “Elston-Ellis histopronostic” grade).
- Grade I: the tumor is not very aggressive.
- Grade II: the tumor is intermediate. This is the most frequent case.
- Grade III: the tumor is aggressive.
The determination of biological markers
The pathologist then analyzes the biological markers (biomarkers) on the surface of the cancer cells. These biological characteristics help to determine the type of cancer and the most appropriate treatment for the patient.
Determination of hormone receptors. If the cancer cell has hormone receptors for estrogen and/or progesterone, the tumor is said to be hormone sensitive. An appropriate treatment (hormone therapy) will then be proposed.
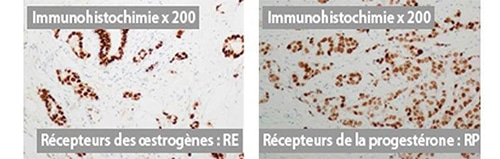
Determination of HER2 status. This protein is involved in cell proliferation. In case of HER2 overexpression (too much of this protein on the cancer cells), postoperative treatment with anti-HER2 is possible (e.g. trastuzumab, whose commercial name is Herceptin®, pertuzumab, etc.). This is called “targeted therapy” because it acts selectively on cancer cells that carry the receptor.
Measurement of the Ki-67 protein index. This protein is a marker of cell proliferation. As for other biomarkers, its study allows to characterize the cell, and can help to choose the best therapeutic strategy.
The final diagnosis
The pathology report gives the characteristics of the tumor:
- The size of the tumor
- The safety margin (measurement of the area of normal tissue around the tumor)
- Type of cancer (ductal, lobular, other)
- Its invasive or in situ character
- Cancer grade, or Elston-Ellis histopronostic grade;
- The presence or absence of hormone receptors, with the percentage of cells that have hormone receptors
- HER2 status (overexpression or not)
- The Ki-67 index to specify the speed of division of cancer cells
- And many other parameters…
The conclusions of the anatomopathological examination constitute the “identity card” of the cancer. They are fundamental in defining the choice of treatments.


Laissez votre commentaire