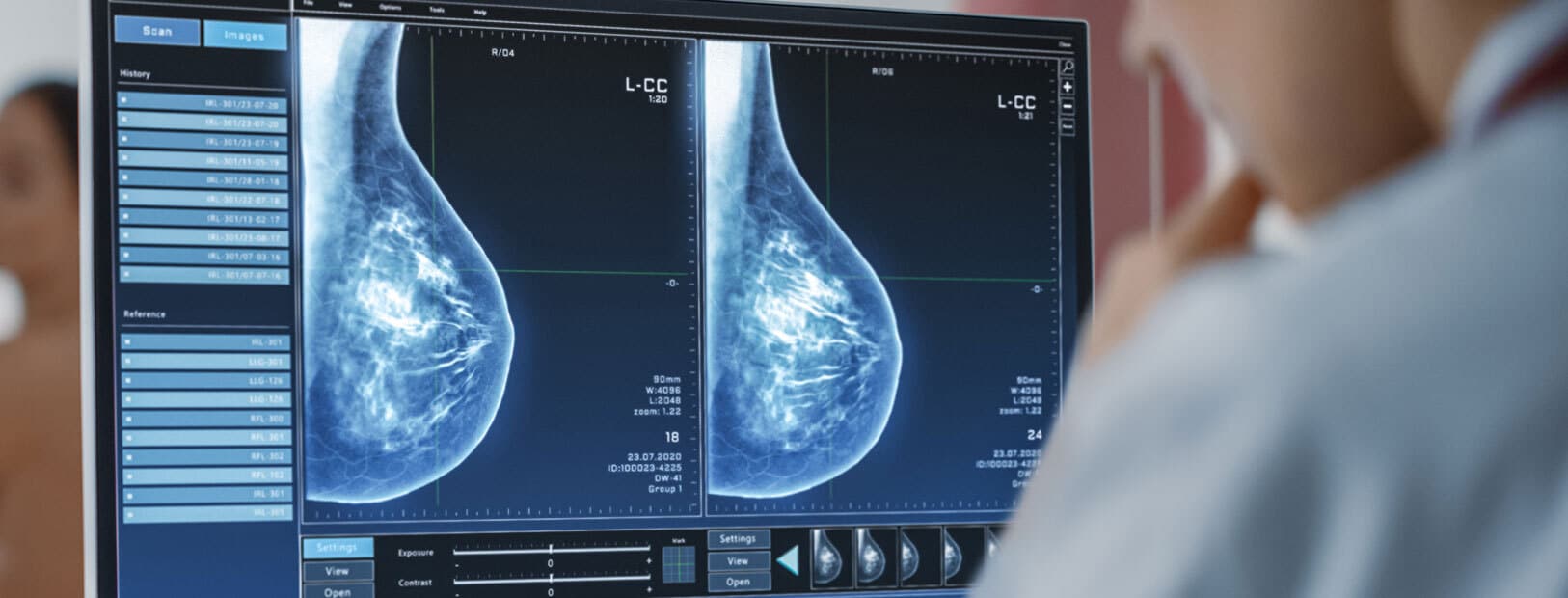
Breast cancer screening
Screening makes it possible to detect cancer early. It increases the chances of recovery and reduces the burden of treatment.
It is recommended that a health professional perform a breast palpation every year from the age of 25.
The age at which you start having mammograms depends on your risk factors for breast cancer. If there is no particular risk, the French National Authority for Health recommends that you have a mammogram every 2 years starting at age 50.
Screening saves lives!
Book an appointment
Dépistage
Dr Krishna B. Clough
Chirurgie cancérologique – Chirurgie reconstructrice et esthétique
Dépistage du cancer du sein
Dr Anne Sabaila
Chirurgie cancérologique et reconstructrice
Le dépistage du cancer du sein
Dr Claude Nos
Chirurgie cancérologique et reconstructrice
La découverte du cancer
Dr Krishna B. Clough
Chirurgie cancérologique – Chirurgie reconstructrice et esthétique
La consultation d'évaluation du risque
Dr Jenny-Claude Millochau
Chirurgie cancérologique et reconstructrice
Introduction to breast cancer screening
80% of breast cancers are diagnosed after the age of 50, with 50% diagnosed between the ages of 50 and 69. This is why all women aged 50 to 74 are invited to participate in breast cancer screening. The screening program is based on a mammogram every two years, which is a 100% covered by the Health Insurance. A second systematic reading of mammograms judged to be normal is done by a second radiologist for safety reasons.
Of course, breast cancer screening is not harmless and has certain disadvantages, including anxiety, “false alarms” following an abnormal examination when there is no cancer found, and even over-diagnosis. However, these disadvantages are largely counter-balanced by the benefits of screening: detected cancers are diagnosed at an earlier stage and benefit from less severe treatment.
Women at high risk
Some women have a much higher than average chance of getting breast cancer. These women are referred to as “high risk”.
These are women:
- who have a personal history of cancer of the breast, uterus and/or endometrium (body of the uterus) or certain breast conditions (atypical hyperplasia or benign proliferative disease);
- who have been exposed to chest radiation before the age of 30, for example for the treatment of Hodgkin’s lymphoma;
- who have a family history of breast and/or ovarian cancer among relatives.
If your risk level for breast cancer is considered “high”, specific monitoring will be offered to you according to your situation and your age. Talk to your doctor: he or she will determine your risk level and suggest the most appropriate monitoring method for your situation.
Risk Assessment Consultation
At the Paris Breast Center we offer a breast cancer risk assessment consultation. You will be seen by a doctor who will quantify your risk according to:
- your personal and family history;
- your radiological examinations;
- a genetic analysis of your individual risk factors.
Following this consultation, we can offer you a customization of your screening, by:
- keeping the same tests as in conventional screening, but starting them earlier and at closer intervals;
- adding other tests to the mammogram, such as an ultrasound or MRI;
- bringing surveillance visits closer together or spacing them out.
The follow-up modalities
No risk factors
An annual clinical examination from the age of 25.
A mammography every 2 years from the age of 50, followed (or not) by an ultrasound.
History of atypical ductal or lobular hyperplasia
An annual mammogram for 10 years, followed (or not) by an ultrasound.
After 10 years:
- the patient is over 50 years old: she is referred to organized screening;
- the patient is less than 50 years old: mammography with or without ultrasound every 2 years until 50 years old.
History of thoracic irradiation (lymphoma, Hodgkin’s, etc.)
A clinical examination and MRI every year, starting 8 years after the end of irradiation.
An annual mammogram (oblique incidence) and a possible ultrasound are recommended.
(No earlier than 20 years for clinical examination and 30 years for MRI).
History of breast cancer
- a clinical examination every 4 to 6 months for the first few years after treatment
- an annual mammogram and ultrasound
- other tests will be determined by your oncologist
At the Paris Breast Center, we offer you a consultation to evaluate your personal risk of breast cancer.
Follow-up arrangements may consist of:
- The same screening tests as in “conventional” screening, but started at a different age and at closer intervals;
- Other detection techniques in addition to or instead of mammography, such as ultrasound or MRI;
- Specific monitoring.
“Very high” risk level / Genetic predisposition to breast cancer
Some genetic predispositions, such as BRCA 1 or BRCA 2 mutations, put women at a “very high” risk of developing breast cancer (an estimated 60%-80% risk of developing breast cancer before age 80).
However, this remains rare: less than 1% of women carry such a mutation. Genetic origin is linked to 5% to 10% of breast cancers.
If your risk of breast cancer is “very high”, you will be monitored in a more specific way: clinical monitoring from the age of 20 and radiological monitoring from the age of 30 (MRI, mammography and ultrasound)
Suis-je concernée ?| Calculation of the Eisinger score and course of action | |
| BRCA1/2 mutation identified in the family………………………..……..5 | Results |
| Breast cancer in a woman before 30 years old…………………….…..4 | 3 or more : |
| Breast cancer in a woman between 30 and 39 years old…………..…..3 | Oncogenetic consultation |
| Breast cancer in a woman between 40 and 49 years old………………2 | Less than 3 : |
| Breast cancer in a man……………………………………………………..4 | Planned Screening |
| Ovarian cancer before age 70……………………………………………………….4 | |
Source : Breast Cancer – Which screening modalities, for which women (InCA, September 2015, available at : https://www.e-cancer.fr/Expertises-et-publications/Catalogue-des-publications/Cancer-du-sein-Quelles-modalites-de-depistage-pour-quelles-femmes)
The level of risk for breast cancer can only be established by a specialist who will decide whether a genetic test is necessary. It is this genetic test that will reveal the possible presence of a predisposing mutation.
However, these mutations are not the only risk factors, and it is necessary to follow the recommended screening procedures according to the patient’s age and risk.







Laissez votre commentaire